 SPINAL CORD EPENDYMOMAS
SPINAL CORD EPENDYMOMAS

Ependymomas are believed to account
for 60% of all primary neoplasms of
the spinal cord and filum terminale.
Intraspinal ependymomas are most
easily grouped into 3 classes:
intramedullary lesions,
myxopapillary ependymomas, and
metastases from an intracranial
origin.
 Preferred
Examination
Preferred
Examination
The initial imaging evaluation
likely includes plain radiography of
the spine. The images may
demonstrate erosion of the pedicle
or scalloping of the dorsal
vertebral body surface. However, the
yield of plain radiography is
limited, and when clinical suspicion
exists, MRI of the spine with and
without gadolinium enhancement is
the study of choice. MRI permits
evaluation of the cord substance
itself for masses and associated
findings such as edema, hemorrhage,
cyst, syringomyelia, and cord
atrophy.
For myxopapillary tumors, both the
brain and spine should be evaluated
with MRI, with and without
gadolinium enhancement. Solitary
intramedullary lesions are less
frequently associated with
intracranial spread; thus, cerebral
imaging is less important.
Myelography may assist in localizing
an intraspinal mass to the
extradural, intradural
extramedullary, or intradural
intramedullary compartments. A
centrally situated, regularly
fusiform cord may be suggestive of
an intramedullary ependymoma,
whereas fusiform swelling in the
cauda equina, particularly when it
is large enough to result in bony
erosion, and a blockage of contrast
enhancement may be consistent with
an ependymoma of the filum.
With a yield similar to those of
plain radiography or myelography,
computed tomography (CT) scan
findings are not conclusive for
ependymoma. Nonspecific findings of
canal widening, bony erosion, and a
thickened cord or filum are
suggestive but not diagnostic of
ependymoma.
 Radiography:
Radiography:
The radiographic diagnosis of
intraspinal tumors is indirect and
nonspecific. Changes induced by the
tumor may be observed in the
adjacent tissues on plain films. The
pedicles may appear eroded,
flattened, or concave, with an
increased interpedicular distance as
a result of chronic pressure
resulting in bony atrophy.
Similarly, scalloping of the
posterior part of the vertebral
bodies or thinning of the lamina
with a widened spinal canal may be
observed. Scoliosis may be visible
on plain radiographs. Finally, in
rare cases, intratumoral
calcification may be observed on
radiographs. Because of the limited
yield of plain radiography, when
clinical suspicion exists, MRI of
the spine with and without
gadolinium enhancement is the study
of choice.
 MRI:
MRI:
On T1-weighted images, ependymomas
generally appear isointense relative
to the normal cord, although they
may appear hypointense (a less
common finding). Heterogeneity and
hyperintensity on T1-weighted images
may indicate a hemorrhagic component
of the mass. On T2-weighted images,
ependymomas are generally
hyperintense relative to the normal
cord. Ependymomas are homogeneously
and intensely enhancing with the
administration of a gadolinium-based
contrast material. With contrast
enhancement, the tumor often is seen
to have well-defined borders.
 Hemosiderin
Hemosiderin
Hemorrhage or hemosiderin in or at
the cranial or caudal margin of
ependymomas is a common imaging
finding. T2-weighted MRIs may
demonstrate a low-signal-intensity
rim around some tumors; this finding
represents the hemosiderin. In 1995,
Fine et al noted this finding in
only 20% of tumors; this percentage
is far lower than the 64% Nemoto et
al reported in 1992.] This
hemosiderin cap is fairly suggestive
of ependymomas. With filum
ependymomas, hemorrhagic products
may be seen within the filum.
 Cysts
Cysts
In 1995, Fine et al observed that 1
of 25 tumors evaluated was cystic,
but 14 had associated reactive
cysts: 11 cysts were rostral to the
tumor; 10, caudal to the tumor; and
7, both rostral and caudal. All
reactive cysts had signal intensity
similar to that of CSF. The cysts
were hypointense on T1-weighted MRIs
and hyperintense on T2-weighted
MRIs. These cysts did not enhance
with the administration of contrast
material. In 1995, Wippold et al
examined 20 patients with
myxopapillary ependymomas; of these,
3 had cystic tumors, and 2 had a
syrinx. Rarely do the tumors
themselves have a cystic appearance.
 Tumor size and location
Tumor size and location
Cervical lesions average 4.2
vertebral segments in length,
thoracic lesions average 3.1
segments, and filar tumors average
4.0 segments. Most often,
intramedullary ependymomas occur in
the cervical cord; fewer lesions are
thoracic, and fewer still occur at
the conus. About 50% of intraspinal
ependymomas occur at the cauda
equina (see the image below); these
are predominantly of the
myxopapillary subtype. Multiple
lesions occur much more often in
this region, with a frequency of
15%.

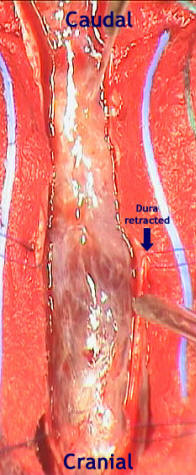
T2-weighted magnetic resonance image
demonstrates a myxopapillary
ependymoma in the cauda equina and
the lesion after dural opening.
 Differential Diagnosis
Differential Diagnosis
The chief intramedullary lesions
from which ependymomas must be
distinguished are astrocytomas and
hemangioblastomas.
Ependymomas of the filum must be
distinguished from schwannomas,
hemangioblastomas, and astrocytomas.
Astrocytomas of the cord are
infiltrative and have margins that
are less sharp than those of the
other lesions. Astrocytomas are less
prone to hemorrhage and infrequently
result in a hemosiderin cap. More
often, astrocytomas are eccentric in
location. Schwannomas may
demonstrate a central area of poor
enhancement.
Hemangioblastomas have prominent
vascularity, as well as large
reactive cysts, which are consistent
with their intracranial appearance.
With MRI, signal intensity
characteristics of hemangioblastomas
are similar to those of ependymomas.
The tumor nodule, which is situated
on a pial surface, may have more
intense enhancement than that of
ependymomas. Local edema of the cord
is more impressive around
hemangioblastomas than ependymomas.
Flow voids are often visible in
hemangioblastomas.
It may be impossible to distinguish
schwannomas from filum ependymomas;
their signal intensity
characteristics are very similar. In
fact, the signal intensity
characteristics of schwannomas and
ependymomas are nearly identical on
T1-weighted, T2-weighted, and
gadolinium-enhanced MRIs.
Schwannomas more often assume a
dumbbell configuration and result in
an enlargement of the adjacent
neural foramina. When the tumors are
small, the observation of an origin
from a root in the cauda equina,
rather than the filum, may aid in
distinguishing schwannomas from
myxopapillary ependymomas. The
distribution of the roots of the
cauda equina in the thecal sac may
help in distinguishing the tumors:
An ependymoma of the filum pushes
the roots to the periphery of the
thecal sac, whereas a schwannoma of
the cauda more often pushes the
roots together in an eccentric
fashion.
Compared with ependymomas,
schwannomas infrequently appear
multilobulated. The periphery of
schwannomas is strongly enhancing,
but the tumors may have central
areas with poor enhancement.
 Note on gadolinium
Note on gadolinium
Gadolinium-based contrast agents
(gadopentetate dimeglumine
[Magnevist], gadobenate dimeglumine
[MultiHance], gadodiamide
[Omniscan], gadoversetamide
[OptiMARK], gadoteridol [ProHance])
have been linked to the development
of nephrogenic systemic fibrosis
(NSF) or nephrogenic fibrosing
dermopathy (NFD). The disease has
occurred in patients with moderate
to end-stage renal disease after
being given a gadolinium-based
contrast agent to enhance MRI or MRA
scans.
NSF/NFD is a debilitating and
sometimes fatal disease.
Characteristics include red or dark
patches on the skin; burning,
itching, swelling, hardening, and
tightening of the skin; yellow spots
on the whites of the eyes; joint
stiffness with trouble moving or
straightening the arms, hands, legs,
or feet; pain deep in the hip bones
or ribs; and muscle weakness.
 Treatment:
Treatment:
Surgical
resection is the choice and it is
limited with the invasive character
of the tumor, but the exophytic
parts can be removed and it is
preferable to use neuronavigation to
avoid damage to the neural
structures. Radiotherapy must
follow with all stages of the
ependymoma.
For
demonstration for a case with filum
terminal ependymoma with exophytic
growth down the cauda equina case
click here!
|